What is breast cancer?
Breast cancer is a type of cancer that disrupts the cell division process in breast cells. Breast cancer cells in a person with the disease multiply uncontrollably and more than they should. There are different types of breast cancer. The type depends on which type of breast cell is affected. The cancer can start in different places in the breast.
The breast has three main parts:
• Lobules: glands where milk is made.
• Ducts: tubes that carry milk from the lobule to the nipple.
• Connective tissue: fibrous and fatty tissue that surrounds and holds the other parts of the breast together.
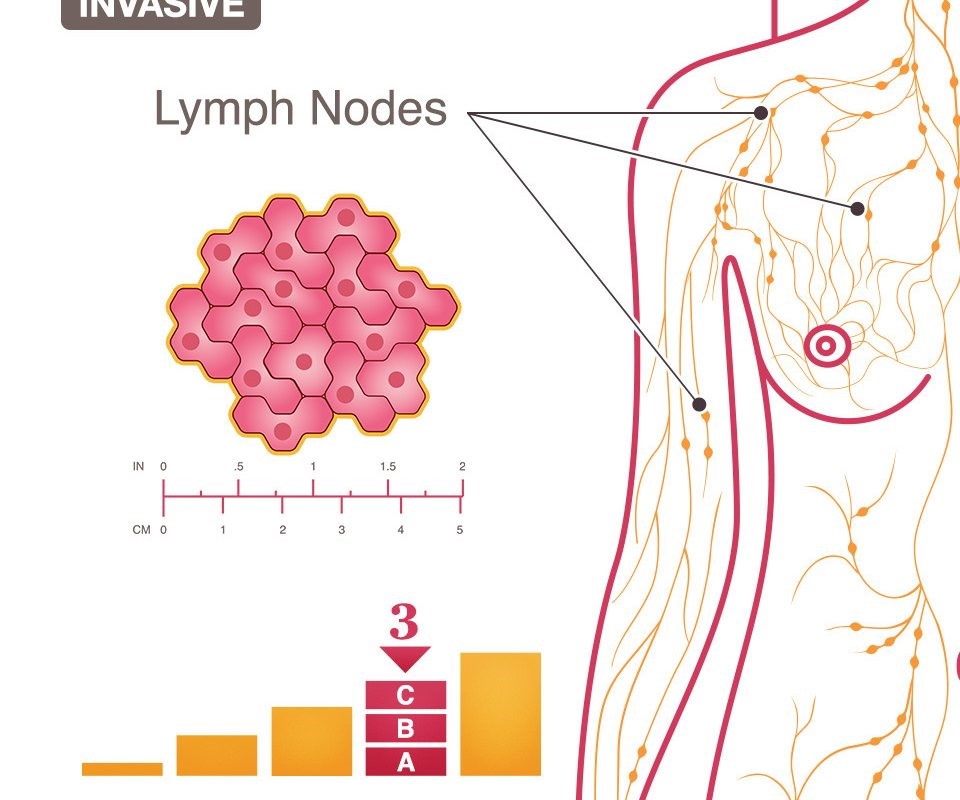
Most breast cancers start in the ducts or lobules. Cancer cells can travel outside the breast through blood vessels and lymph channels and spread to the rest of the body. In this case, we say that the cancer has metastasized.
What are the different types of breast cancer?
The most common types of breast cancer are:
• Invasive ductal carcinoma: In this type of breast cancer, cancer cells form in the ducts. After progressing, they gradually move outward and reach other parts of the breast. These cells may even break out of the breast and affect other areas of the body.
• Invasive lobular breast cancer: In this type of cancer, cancer cells first form in the lobules and then move to the rest of the breast and beyond.
There are other types of breast cancer that are not as common, such as Paget's disease, medullary carcinoma, mucinous carcinoma, and inflammatory breast cancer.
Assessment
Take a complete health history
Assess the patient's response to the diagnosis and ability to adapt
Ask about coping skills, support systems, lack of awareness, and presence of discomfort.
Preoperative nursing diagnoses
Lack of awareness about the intended surgical treatment.
Anxiety related to the cancer diagnosis
Fear and relationship to specific treatments, changes in body image.
Risk of ineffective adjustment (individual or family) related to the diagnosis of breast cancer and treatment methods.
Conflict in decision-making
Postoperative nursing diagnoses
Pain and discomfort related to the surgical procedure
Impaired decision-making related to nerve stimulation in the affected arm, chest, or thorax.
Impaired mental image related to changes in the breast as a result of surgery.
Adjustment disorders related to cancer diagnosis and surgical treatment.
Deficits in self-care related to immobility of the upper limb on the side of surgery.
Risk of sexual dysfunction related to loss of a body part, changes in self-image, and fear of the spouse's response.
Lack of knowledge regarding drain control after breast surgery.
Lack of knowledge regarding open exercise and to restore movement in the operated limb.
Lack of knowledge regarding arm care immediately after total mastectomy.
Provide education and preparation about surgical treatment
Review treatment methods with emphasis on information previously given to the patient and answer the patient's questions.
Fully prepare the patient for what will happen before, during, and after surgery.
Inform the patient that there will be reduced mobility in the arm and shoulder area after total mastectomy and that the patient should be able to move these two joints through their range of motion before discharge.
Reassure the patient that painkillers and other methods of pain relief will be available.
Reduce fear and anxiety and improve coping skills
Help the patient come to terms with the physical and emotional effects of the disease.
Guide the patient about realistic expectations for their recovery process, thereby reducing the patient's fears (fear of pain, fear of not being able to care for themselves and their family).
Inform the patient about available support resources (such as a cancer society, social worker, psychologist, and support groups). Talking to someone else who has had breast cancer and has undergone treatment similar to the patient's may help the patient.
Promote decision-making skills
Help the patient and family evaluate the risks and benefits of each proposed treatment.
Ask the patient questions about each treatment option to help her choose the best treatment for her (e.g., How do you feel about losing your breast?
Have you considered breast augmentation? If you want to keep your breast, can you tolerate radiotherapy up to 5 days a week for 5 to 6 weeks?)
Support any decisions the patient makes. Postoperative Nursing Interventions
Pain and Discomfort Relief
Assess the patient carefully for pain. Each person responds differently to pain. Encourage the patient to take painkillers.
Inform the patient that there may be an increase in pain after the first few days as sensation returns to the surgical site and as the patient increases in activity.
A patient who complains of pain should be carefully evaluated for possible complications of surgery, such as infection or hematoma.
Offer the patient a variety of pain management techniques (e.g., warm baths, distraction, guided imagery).
Control post-surgical sensations
Assure the patient that post-surgical sensations (e.g., tenderness, hypersensitivity, pain, numbness, tingling, pulling, twisting, and phantom sensations after mastectomy) are a normal and expected part of the healing process and do not indicate a problem.
Promote a positive body image
Increase the patient’s awareness of the surgical incision site to